Have you ever experienced that unsettling feeling in your ear, only to discover it’s caused by fungi? Yes, “hongos en el oído” can be a surprising yet common issue, affecting many people more than you might think. Understanding the main causes and effective treatments for this condition is essential in regaining your comfort and health. In this article, we’ll explore the underlying factors contributing to ear fungal infections, as well as the most effective remedies to help you tackle this pesky problem head-on. Let’s dive into the world of ear health and uncover the information you need to stay informed and feeling great!
Understanding Ear Fungi Symptoms
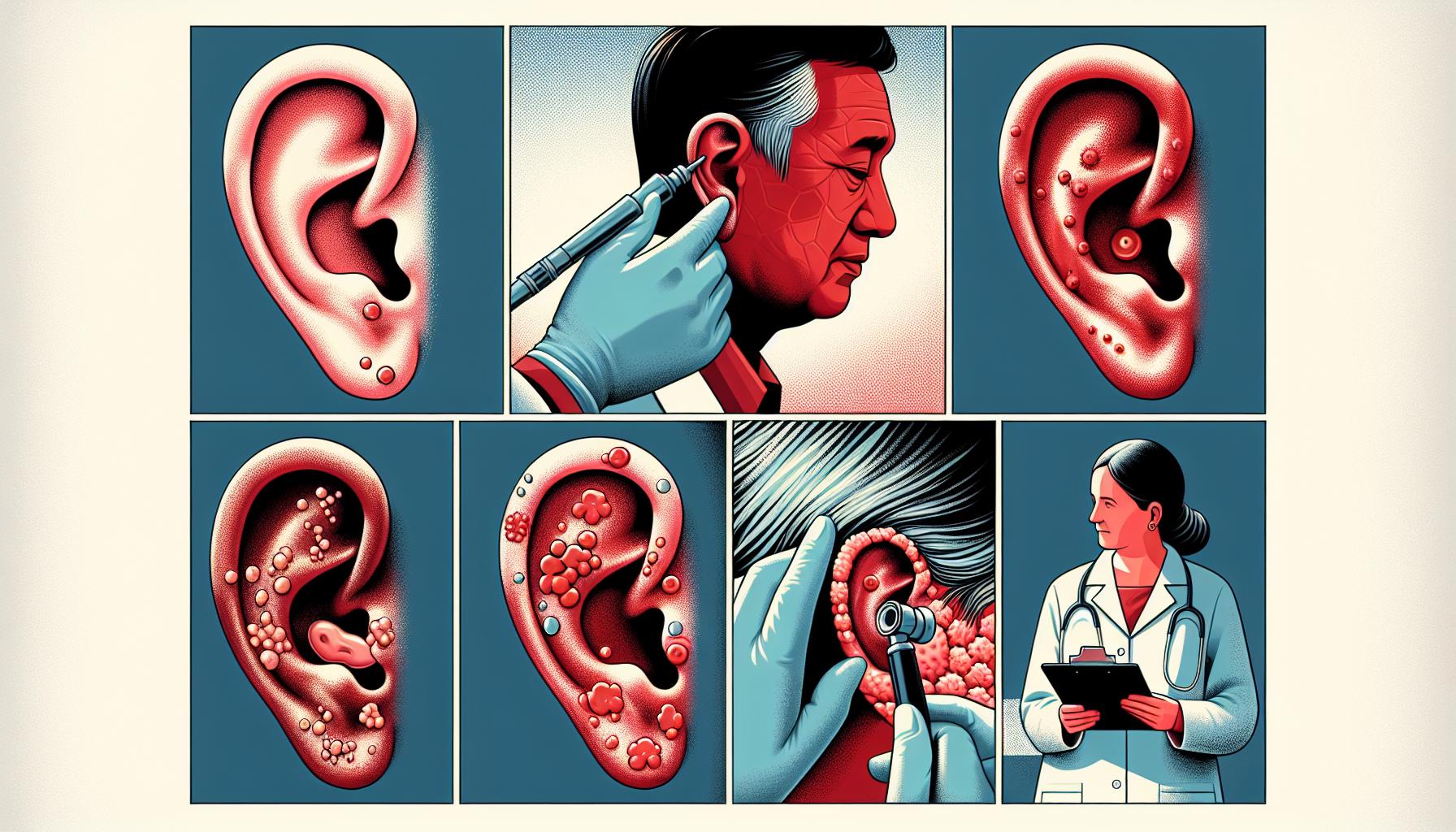
When it comes to ear fungi, it’s essential to recognize the pesky symptoms before they turn into a full-blown party—one you definitely won’t want to attend. Often, individuals might chalk up ear discomfort to wax buildup or allergies, but when fungi join the fray, the signs can take a turn for the creepy and unusual. So, what should you keep your eye on? Let’s dig into the notable indicators that may signal a fungal invasion in your ear.
Common Symptoms to Watch For
Imagine your ear as the cozy living room of your favorite coffee shop— when it’s clean and tidy, everything runs smoothly. However, introduce some uninvited guests like fungi, and things can get pretty chaotic. Here are some symptoms that might hint at the presence of ear fungi:
- Itching or irritation: One of the first red flags, like a persistent itch that just won’t let you enjoy your day. If it feels like tiny ants are having a dance party in your ear, it’s time to pay attention.
- Pain or discomfort: While not everyone experiences this, some might feel a dull ache or sharp pain, reminiscent of that time you bit into a jalapeño thinking it was a cucumber.
- Fluid discharge: If you notice an unusual discharge from your ear, especially if it’s discolored or has a foul odor, think of it like an uninvited guest leaving a stinky mess behind.
- Hearing loss: A temporary drop in your hearing ability can happen, akin to watching your favorite action movie with the sound turned to zero.
Spotting the Differences
It’s easy to confuse ear fungi with other conditions affecting the ear. Think of it like mistaking a chai latte for a pumpkin spice—both delicious, but definitely not the same! Here’s a quick comparison to help you differentiate:
| Symptom | Fungal Infection | Earwax Buildup | Ear Infection |
|---|---|---|---|
| Itching | Common | Less Common | Rare |
| Pain | Possible | Unlikely | Very Common |
| Fluid Discharge | Possible | No | Often |
| Hearing Loss | Can occur | Common | Common |
Staying aware of these symptoms can make a world of difference in early diagnosis and treatment. In case you suspect ear fungi, don’t hesitate to consult a healthcare professional. They’ll equip you with the right tools and advise on how to kick those unwelcome guests out for good! Like any sequel of a bad movie, you don’t want to end up facing the same problem again and again!
Uncovering Common Causes of Ear Fungi
Ear fungi can be a perplexing nuisance, lurking in the shadows and waiting for the perfect moment to unleash their itchy, sometimes painful presence. While life might throw many curveballs our way, don’t let fungi get you down! Understanding the common causes of these pesky intruders can help you sidestep their unwelcome visits.
Moisture and Humidity
One of the primary culprits behind ear fungi is simply moisture. Think about it: your ears are like little rainforests. If you spend too much time swimming, showering, or just living in a humid climate, fungal growth can flourish. They thrive in dark, damp places—kind of like that laundry pile you keep forgetting about. Consider this: our ears aren’t designed to handle excess moisture, making them prime real estate for unwanted guests.
- Swimming or bathing frequently: Water can linger in the ear canal, creating that perfect breeding ground.
- Excessive sweating: Sure, summer’s great for beach days, but the sweat can lead to a moisture imbalance.
Underlying Skin Conditions
Some underlying skin conditions can also pave the way for fungi. Think of eczema or psoriasis as the uninvited chores that invite messy fungi to your ear canal party. These conditions can disrupt the skin’s protective barrier, allowing fungi to take over like the overly friendly neighbor who overstays their welcome.
- Eczema: Flaky, itchy skin? Fungi love those skin cells.
- Dermatitis: Inflammation can compromise the skin’s defense, making it easy for fungi to join the fun.
Weakened Immune System
A weakened immune system is akin to a castle without its walls; it leaves you vulnerable. Stress, illness, and poor nutrition can all lead to a compromise in your body’s defensive army. When you don’t feel your best, fungi can do their happy dance through your ear canal, practically throwing a disco party.
- Stress: It’s like inviting a storm cloud into your brain. Stress hormones can weaken immune responses.
- Chronic conditions: If chronic illnesses are part of your life’s menu, your immune system may not be at its strongest.
Inadequate Ear Hygiene
While it might seem counterintuitive, poor ear hygiene can contribute to fungal infections. Over-cleaning or sticking foreign objects in your ears might strip away natural oils and irritate the skin. It’s like trying to paint a masterpiece on a canvas that’s constantly getting wiped clean — no wonder it gets confusing!
- Q-tips misuse: These handy little tools can actually push wax deeper or irritate the skin, leading to issues.
- Not drying your ears properly: Remember to gently towel-dry your ears post-shower or swim—think of it as keeping your little rainforests from turning into swamps.
Ultimately, while ear fungi may be a common inconvenience, a keen understanding of their roots can help keep them at bay. Keeping moisture levels in check, managing skin conditions, supporting your immune health, and practicing good ear hygiene can create an unwelcoming environment for fungi, steering them away from your ears and back into the shadows.
Effective Treatments for Ear Fungal Infections
Fungal infections in the ear can feel a bit like a bad relationship; they start off quietly enough but soon they’re all you can think about! If you’re dealing with discomfort, itching, and perhaps a strange discharge, it’s probably time to get savvy about effective treatments. Thankfully, there are a variety of options that can lead you towards relief. Here are some solid approaches you might consider.
Medications & Topical Treatments
Over-the-counter and prescription medications can be a game-changer. Antifungal ear drops like clotrimazole or miconazole can quickly tackle those unwelcome guests in your ear canal. You just apply a few drops, and it’s like sending in the special forces! You may even find some products that combine antifungals with steroids to reduce inflammation — talk about a double whammy!
For those who prefer a more holistic approach, natural remedies can also provide relief. Some folks swear by apple cider vinegar diluted in water to restore pH balance, while others rely on garlic oil for its antifungal properties. Just make sure you’re not using anything too strong that could irritate your ears further! A good rule of thumb is to consult with a healthcare professional before trying DIY solutions, especially if you’re unsure.
Cleaning & Drying Techniques
Keeping your ears dry is vital in managing fungal infections, as moisture creates a perfect breeding ground for those pesky fungi. You might consider using a hair dryer on a low setting, keeping it at a safe distance (no one wants fried eardrums), or simply tilting your head to let any water escape after showering. Cotton swabs can be tempting, but use them sparingly — they often push wax deeper instead of removing it!
Consider incorporating a regular ear cleaning routine. A gentle saline solution can effectively flush out debris without causing irritation. Just mix a teaspoon of salt in a cup of warm water, and you’ve got yourself a simple yet effective ear rinse.
When to Seek Professional Help
If home remedies aren’t cutting it, don’t hesitate to reach out to a healthcare professional. Persistent pain or symptoms that worsen could indicate a more severe infection or even a secondary bacterial infection. You’ll want to have those checked out before they snowball into something more serious!
Taking probiotics may also help in supporting overall ear health; some studies suggest that they can help balance the body’s natural flora, which could mean fewer ear infections over time. While research is still ongoing, the connection between gut health and ear health is starting to make waves in the medical community.
At the end of the day, dealing with ear fungal infections can feel daunting, but the right combination of treatments could turn your squeaky situation around. Keep your ears dry, remain informed about effective medications, and don’t shy away from professional advice when needed!
Preventive Measures for Ear Fungus
When it comes to keeping ear fungus at bay, a bit of forethought goes a long way. You know what they say: an ounce of prevention is worth a pound of cure! Just like avoiding overly spicy tacos before a big meeting (or a first date), there are some straightforward strategies you can implement to help maintain happy, fungus-free ears.
Protect Your Ears From Moisture
Moist environments are a fungi’s paradise, so keeping your ears dry is crucial:
- Swim Smart: Use earplugs or a swim cap if you’re diving into the pool or the ocean. Better safe than sorry, right?
- Dry Off: After showering or swimming, gently dry your ears with a towel. Avoid sticking anything into your ear canal—no Q-tips or forgotten pencils!
- Avoid Over-Cleaning: Your ears produce natural wax, which serves as a barrier. Don’t go on a cleaning rampage; instead, let nature do its thing.
Check Your Environment
Have you ever noticed a bit of humidity in your home that feels like a tropical rainforest? Well, that’s not just a bad hair day; it’s also a potential breeding ground for ear fungi. Consider taking the following steps:
- Control Humidity: Invest in a dehumidifier if your home feels like a sauna. Keeping humidity levels under 50% can help reduce pesky fungal growth.
- Avoid Sharing Hygiene Products: Sharing personal items like earbuds or hairbrushes can be a fungus-free-for-all! Keep your ear gear to yourself.
Mind Your Ear Health
Just like keeping up with your dentist appointments (and that mid-year New Year’s resolution), taking care of your ear health is vital:
- Regular Check-ups: If you have a history of ear infections or issues, don’t skip those annual check-ups. Your doctor can spot problems before they escalate.
- Address Allergies: Allergies can increase inflammation in the ears, creating an environment ripe for fungi. Talk to a healthcare professional about managing your symptoms.
Be Mindful of Your Diet
Believe it or not, what you put into your body can influence ear health:
- Stay Balanced: A balanced diet rich in vitamins (especially vitamins C and E) and minerals can boost your immune system, helping to fight off infections.
- Limit Sugar: High sugar levels may encourage fungal growth, just like how old pizzas attract glittering cockroaches! Reducing sugar can help keep those fungi at bay.
Remember, while these tips can significantly reduce your risk of ear fungus, they’re not foolproof. Staying informed, being aware, and asking questions can empower you on this journey for better ear health. Keep your ears clean, dry, and happy, and they’ll sing your praises—well, metaphorically, at least!
When to Seek Professional Help
When you’re grappling with the discomfort of ear fungus, it can often feel like you’re stuck in a never-ending battle. You may be trying to ignore it, hoping that it will just “go away” like that weird smell in the fridge you’re avoiding addressing. But some problems need more than just a solid dose of optimism. Seeking professional help can be a necessary step when things escalate past simple irritation.
Recognizing the Signs
Identifying when to pull the trigger and go see a professional can feel like deciphering Morse code through static. But there are key signs that should help you make that decision:
- Persistent Pain: If your ear feels like it’s hosting its own heavy metal concert, and no amount of over-the-counter pain relief is cutting through that discomfort, it’s time to talk to a doctor.
- Discharge: Any weird, funky discharge from the ear is a red flag. While everyone has their “off days,” if your ear looks like it’s joined a punk band, it’s a call for medical intervention.
- Hearing Loss: If your world seems to be getting quieter and quieter, or you’re asking people to repeat themselves more than a neighbor’s parrot, get checked out.
- Recurrence: If you keep having these pesky fungi crashing in after every treatment, you might need a deeper dive into the issue.
What to Expect at the Doctor’s
When you finally decide to go for a check-up, know that the process isn’t as daunting as it seems. Typically, you’ll start with a thorough examination by an ENT (ear, nose, and throat specialist). They might use an otoscope—a fancy tool that looks like something from a sci-fi movie—to get a good glimpse inside. Expect questions that will cover everything from your recent history of ear infections to your favorite swimming spots. This information helps them tailor the treatment more effectively.
Then, depending on their findings, they may recommend one of several treatment options, including antifungal medications or even a customized cleaning regimen. And don’t be shocked if they suggest you ditch some of your cotton swab habits; it turns out they can push debris further into the ear canal rather than cleaning it. Just like that one friend who thinks they can “fix” your love life by introducing you to their cousin Greg.
The Importance of Listening to Your Body
remember that your body is your best friend in situations like this—it often whispers (or screams) cues about what’s wrong. Feeling in tune with your body is a key part of knowing when to pull the trigger on medical assistance. By understanding the signals it sends, you become not just a patient but an active participant in your health journey.
Here’s a handy-dandy comparison table to summarize when seeking help is a must:
| Symptoms | Seek Professional Help? |
|---|---|
| Persistent pain despite over-the-counter treatments | Yes |
| Any unusual discharge | Yes |
| Significant hearing loss | Definitely Yes |
| Frequent recurrence of symptoms | Absolutely Yes |
By knowing when to get professional help, you can feel empowered to tackle ear fungus head-on, instead of feeling like it’s a game of Whack-a-Mole with your health.
Debunking Myths About Ear Fungi
When it comes to fungi in the ears, there’s a treasure trove of myths floating around like wayward mushrooms. It might feel tempting to believe everything you hear—like thinking ear fungi are just a figment of a doctor’s imagination or that only the unclean suffer from these pesky invaders. Hold onto your hats, folks! It’s time to sift through the garden of misinformation and get to the juicy roots of the truth.
The “It’s Just a Dirty Ear” Myth
Let’s bust the myth that only filthy ears play host to fungi. Sure, maintaining proper hygiene is crucial; however, fungal infections can decide to crash your ear party regardless of how nifty your cleaning routine is. Factors such as moisture, humidity, and even certain health conditions like diabetes can invite these fungi over for a prolonged stay. So, if you thought you were immune because you scrub a little harder than most, think again!
Just last week, my buddy Mark, a self-proclaimed cleanliness fanatic, treated himself to a sauna. A few days later, he had a severe case of ear fungi! Turns out, that steamy environment was fungus’s version of an all-you-can-eat buffet. Not exactly appealing, right?
Another common misconception is that if your ear hurts, it must be due to pesky fungi. While ear pain can be a symptom, it doesn’t exclusively indicate a fungal issue—plenty of other conditions can cause that discomfort. For instance, wax build-up, bacterial infections, or even sinus problems can play the villain in ear health. Yes, fungi can be guilty, but don’t forget about the entirely innocent bystanders!
Imagine this: you’ve got a sore ear, and your first instinct is to blame the cheeky fungi. Rushing to treat it can sometimes lead you to apply the wrong remedy—like applying the sprinkle of fairy dust that was meant for cleaning (yep, happened to my friend Lucy). A professional diagnosis is crucial here. Trust me, seeing a healthcare provider could save you from a DIY disaster!
Many people assume that having fungi in the ear is a life-threatening situation straight out of a horror movie. While it can be uncomfortable and needs addressing, in most cases, it’s manageable with proper treatment. Though some fungal infections, like otomycosis, can be persistent, they typically don’t pose serious health threats if treated promptly.
Of course, don’t ignore it altogether! Left unchecked, a simple case of ear fungi could lead to secondary infections which are no joke. It’s always better to tackle it before it decides to settle down permanently. Keep in mind that not all heroes wear capes; sometimes they just wear scrubs and carry otoscopes!
Many folks swear by home remedies, but relying solely on DIY treatments for ear fungi can lead you to dance on the edge of a razor blade. While garlic oil and tea tree oil might work wonders for some, these alternatives are not failsafe. There’s a fine line between enhancing your ear health and inviting trouble. Using improper substances can exacerbate the condition or cause irritation. Remember that friend who tried to treat their ear with vinegar and ended up feeling like they were hosting an angry bee party? Yeah… don’t be that friend.
In short, while hearing some myths can be amusing like a good sitcom, they can also mislead you when it comes to health. Educate yourself, don’t let your ears be a playground for unfounded assumptions, and when in doubt, feel free to consult a healthcare professional. Your ears will thank you later, even if they might be a little sneaky sometimes!
Navigating Recovery from Ear Fungus
Dealing with ear fungus can feel like a unique kind of struggle, almost like getting a mosquito bite in a spot you can’t reach. Trust me, you’re not alone if you suddenly find yourself feeling a bit perplexed. First things first, let’s clear the air—ear fungus isn’t something that pops up out of nowhere! It often thrives in dark, moist environments, and if you’ve been enjoying the pool a little too much or indulging in a bit of excessive earwax harvesting, you might be giving these pesky spores a VIP pass to your inner ear.
What to Expect During Recovery
Recovery from ear fungus may seem like a marathon rather than a sprint, but armed with the right mindset and tools, you can make it through. Antifungal medications are typically your best buddies here. These might come in the form of ear drops or pills, depending on the severity of your case. Keep a sharp eye out for symptoms like itching, discharge, or a sensation akin to a tiny drummer playing in your ear—you’ll want to loop your healthcare provider in if these sensations escalate. It’s important to remember that while some folks might see improvement quickly, others could take a bit longer, which can feel as frustrating as waiting for your favorite band to release a new album.
Practical Tips for Managing Symptoms
Here’s where some practical wisdom comes into play. If your ear feels stuffy or clogged, resist the urge to dig around—trust me, no one wants to end up with a surprise ear injury on top of everything else! Instead, consider these tips to ease your path to recovery:
- Keep your ears dry: Consider wearing earplugs while swimming or showering. A little extra diligence can help prevent excess moisture.
- Avoid irritants: Steer clear of cotton swabs and other tools that do more harm than good. Use a soft, damp cloth to clean the outer ear, but leave the inner parts alone.
- Boost your immune system: Eating a balanced diet rich in vitamins can help your body fight off those fungal foes. Think fruits, veggies, and whole grains.
Understanding Your Treatment Options
Now, let’s chat a little about your treatment options. The most common antifungal medications include clotrimazole and nystatin; both have been shown to clear infections effectively. If you’re into reading labels, you might find them in formulations like creams or solutions. Here’s a simple breakdown of what these treatments can do for you:
| Medication | Form | Frequency | Side Effects |
|---|---|---|---|
| Clotrimazole | Solution/Drops | 2-3 times a day | Itching, redness |
| Nystatin | Suspension/Drops | 2-4 times a day | Gastrointestinal issues in rare cases |
While these medicines are often safe and effective, always chat with your healthcare provider first. It’s like getting a second opinion on whether ‘that’ outfit looks good on you—crucial for making the right choice! There’s also ongoing research focusing on newer antifungal options, which may offer better-targeted treatments with fewer side effects, so keep an eye on the horizon!
Navigating recovery doesn’t have to feel like a frustrating maze. With the right treatments, self-care practices, and a bit of patience, you’ll be back to your usual self before you can say “ear infection.” Just remember, everyone’s journey is unique, and finding what works best for you might take a little experimentation.
Frequently asked questions
What are the primary causes of fungal infections in the ear?
Fungal infections in the ear, commonly referred to as otomycosis, can stem from various factors. One of the most significant causes is excess moisture in the ear canal. Environments such as swimming pools, lakes, and even excessive sweating can create ideal conditions for fungi to thrive. According to a study published in the Journal of Otolaryngology, approximately 80% of otomycosis cases are linked to water exposure. This is particularly relevant for individuals who enjoy water sports or have a habit of using cotton swabs, which can inadvertently push moisture deeper into the ear.
Other factors contributing to fungal infections include compromised immune systems and underlying skin conditions, such as eczema or psoriasis, which can create an environment conducive to fungal growth. Additionally, the use of certain medications, especially antibiotics, can disrupt the natural balance of flora in the ear, allowing fungi to proliferate unchecked. Studies show that prolonged antibiotic use can lead to higher instances of fungal infections, with some reports citing that as many as 30% of patients develop otomycosis following a course of antibiotics.
How can you identify the symptoms of a fungal ear infection?
Recognizing the symptoms of a fungal ear infection is crucial for timely intervention and treatment. Common signs include itching, discomfort, and a feeling of fullness in the ear. Patients may also experience a sensation similar to that of water trapped in the ear. Another hallmark of otomycosis is the presence of a black or white discharge, which can sometimes be mistaken for earwax but indicates the presence of fungal hyphae or spores.
In more severe cases, symptoms can escalate to include pain, redness, and swelling in the ear canal. If the infection spreads, individuals may experience hearing loss or even vertigo, leading to unsteadiness. It’s essential to consult a healthcare provider if symptoms persist beyond a few days or worsen, as untreated fungal infections can lead to more serious complications. According to the American Academy of Otolaryngology, early detection can significantly reduce recovery time and prevent further complications.
What effective treatments exist for fungal infections in the ear?
Treating fungal infections in the ear typically involves both antifungal medications and supportive care. Over-the-counter antifungal creams or eardrops can be effective for mild cases. However, in more severe situations, a healthcare professional may prescribe stronger antifungal medications, such as clotrimazole or fluconazole. These help eliminate the underlying fungal infection and restore the ear’s natural balance.
In addition to pharmacological treatments, healthcare providers often recommend keeping the ear dry. This may involve tips like avoiding moisture during bathing or swimming and allowing some time for the ear to air out — never using cotton swabs, which can aggravate the condition. Using a hairdryer on a low, cool setting aimed at the ear (from a distance) is another home remedy some practitioners suggest to help dry the ear canal safely.
How can you prevent fungal infections in the ear?
Preventing fungal infections in the ear revolves largely around maintaining proper ear hygiene and managing moisture levels. One of the most effective strategies is to avoid prolonged exposure to water, especially in environments known to harbor fungi, such as public pools. If swimming is unavoidable, utilizing earplugs or a swim cap can help keep water out of the ear canal.
Another critical preventive measure is to practice good ear hygiene. This includes avoiding the use of cotton swabs inside the ear, as they can push wax and debris deeper and potentially create a breeding ground for fungi. For individuals who are prone to ear infections or dry ear canal environments, regular checks with a healthcare professional can help reduce recurrence risks.
When should you seek medical attention for an ear infection?
While many mild ear infections can resolve on their own, there are certain situations where seeking medical attention becomes imperative. If symptoms such as persistent pain, hearing loss, or significant discharge are present and do not improve within a couple of days, it’s crucial to consult a healthcare provider. Delays in treatment can lead to complications such as chronic infections or, in rare cases, spread to other parts of the ear and head.
Moreover, anyone with a compromised immune system, such as those undergoing chemotherapy or living with conditions like diabetes, should be particularly vigilant. Symptoms that include fever, severe dizziness, or swelling beyond the ear itself warrant immediate medical evaluation. The early management of fungal infections is key to a swift and uncomplicated recovery, as delaying treatment can often lead to more complex health issues.
Can lifestyle factors influence the risk of developing ear fungi?
Indeed, lifestyle factors can significantly influence the risk of developing fungal infections in the ear. For example, individuals who frequently engage in water-related activities, such as swimming or diving, are at a higher risk due to increased exposure to water. Additionally, those with habits that contribute to ear moisture—like using earplugs that do not allow for proper ventilation—may find themselves more susceptible to fungal growth.
Furthermore, individual health habits, such as controlling underlying conditions like diabetes, can play a critical role in prevention. A well-managed health regime, with a focus on hygiene and environmental control, can greatly reduce the likelihood of developing otomycosis. For instance, ensuring that any cuts or abrasions in or near the ear are properly cared for helps eliminate potential entry points for fungi. Regular wellness check-ups can also assist in catching early signs of infection before they escalate.
Key Takeaways
understanding “Hongos en el oído: Principales causas y tratamientos efectivos” is crucial for anyone looking to maintain their ear health and avoid the discomfort that comes with fungal infections. Whether you’re a frequent swimmer, a music enthusiast, or simply someone who enjoys a good pair of earbuds, being aware of the symptoms and preventative measures can make all the difference in your auditory experience. Remember, while home remedies might seem tempting, consulting a healthcare professional is essential for effective treatment and to prevent complications.
So, the next time you find yourself scratching that ear (and no, we don’t mean the dance move), you’ll be equipped with knowledge backed by research and real examples to tackle any ear fungi issues head-on. Let’s keep the music playing and those pesky fungi at bay! After all, an earful of fun is better than an earful of fungal!